Introduction
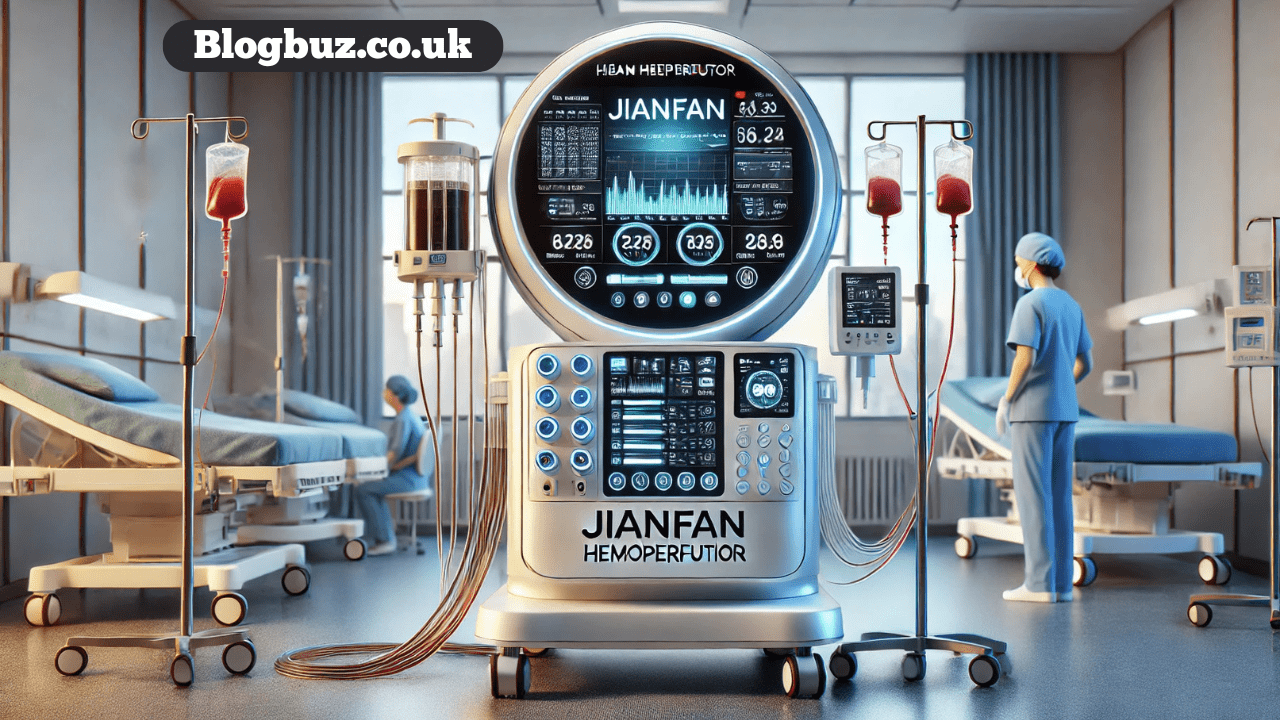
For patients battling severe inflammatory diseases, sepsis, or acute organ injury, the body’s own immune response can become a destructive force. An excessive release of inflammatory mediators, often called a “cytokine storm,” can lead to widespread tissue damage and organ failure. Medical technology has been searching for effective ways to intervene, and one promising innovation in this field is the Jianfan hemoperfutor.
This device represents a significant step forward in extracorporeal (outside the body) blood purification. The primary goal of a hemoperfutor is to filter a patient’s blood, removing harmful substances like inflammatory cytokines, toxins, and metabolic waste. By selectively removing these damaging molecules, the Jianfan hemoperfutor aims to restore balance to the immune system, reduce inflammation, and support organ function, offering a new line of defense for critically ill patients.
This guide will explain what the Jianfan hemoperfutor is, how it works, and its potential applications in modern medicine. We will look at its benefits, the clinical evidence supporting its use, and how it compares to other treatments.
How Does the Jianfan Hemoperfutor Work?
The Jianfan hemoperfutor operates on the principle of hemoperfusion, a medical procedure where a patient’s blood is passed through a device containing adsorbent materials to remove specific toxic substances.
The core of the Jianfan system is a cartridge filled with specialized, biocompatible resin beads. These beads have a unique porous structure and a large surface area, specifically designed to capture and bind targeted molecules from the blood.
The mechanism of action involves these key steps:
- Blood Diversion: The patient’s blood is drawn from a major vein, similar to a standard dialysis procedure, and directed into the hemoperfusion circuit.
- Filtration and Adsorption: Inside the cartridge, the blood flows over the resin beads. These beads act like tiny magnets, selectively adsorbing harmful substances such as inflammatory cytokines (e.g., interleukins, TNF-alpha), endotoxins, and other inflammatory mediators.
- Purified Blood Return: After passing through the cartridge, the purified blood, now with lower levels of harmful substances, is returned to the patient’s circulatory system.
This process effectively “cleanses” the blood of the molecules that drive systemic inflammation, helping to break the cycle of damage associated with conditions like sepsis and acute respiratory distress syndrome (ARDS).
Benefits of Using the Jianfan Hemoperfutor
The primary advantage of using the Jianfan hemoperfutor is its ability to modulate the body’s inflammatory response. Key benefits include:
- Targeted Cytokine Removal: It effectively reduces the concentration of pro-inflammatory cytokines, helping to control the “cytokine storm” and mitigate its damaging effects on organs.
- Improved Hemodynamic Stability: By removing inflammatory mediators, hemoperfusion can help stabilize a patient’s blood pressure and improve cardiovascular function, reducing the need for vasopressor medications.
- Support for Organ Function: Lowering the inflammatory burden can protect vital organs like the lungs, kidneys, and liver from injury, potentially improving patient outcomes and recovery times.
- Safety and Biocompatibility: The materials used in the cartridge are designed to be highly biocompatible, minimizing the risk of adverse reactions or blood cell damage during the procedure.
Applications in Healthcare
The Jianfan hemoperfutor is being explored for a variety of critical care applications where systemic inflammation is a major contributing factor. These include:
- Sepsis and Septic Shock: Sepsis is a life-threatening condition caused by the body’s overwhelming response to an infection. Hemoperfusion can help remove the endotoxins and cytokines that fuel this response.
- Acute Respiratory Distress Syndrome (ARDS): In ARDS, severe inflammation damages the lungs. Reducing cytokine levels may help improve lung function and oxygenation. This application gained significant attention during the COVID-19 pandemic.
- Acute Kidney Injury (AKI): By alleviating the systemic inflammation that can contribute to kidney damage, hemoperfusion may play a supportive role in managing AKI.
- Post-Surgical Complications: Following major surgeries, some patients develop a systemic inflammatory response. Hemoperfusion could be used to manage this complication and improve recovery.
What Do Clinical Trials Say?
Several clinical trials have investigated the efficacy and safety of Jianfan hemoperfusion devices. While results can vary based on the patient population and the specific condition being treated, many studies have shown positive outcomes.
For example, trials involving patients with sepsis have often demonstrated a significant reduction in circulating cytokine levels following treatment. Some studies have also reported improvements in clinical markers, such as better hemodynamic stability and a decreased need for life support. Research conducted during the COVID-19 pandemic suggested that hemoperfusion could be a valuable tool for managing severe cases characterized by a cytokine storm, potentially improving survival rates in critically ill patients.
It is important to note that the medical community is still working to define the optimal timing, duration, and patient selection criteria for hemoperfusion therapy to maximize its benefits.
Potential Risks and Side Effects
Like any medical procedure, hemoperfusion carries potential risks, although they are generally considered manageable. Possible side effects include:
- Thrombocytopenia: A temporary drop in platelet count can occur as blood interacts with the perfusion circuit.
- Hypotension: Some patients may experience a drop in blood pressure during the procedure.
- Clotting: Anticoagulation (blood-thinning) medication is required to prevent clots from forming in the circuit, which carries its own risk of bleeding.
- Infection: As with any procedure involving extracorporeal circuits, there is a small risk of infection at the catheter insertion site.
Medical teams closely monitor patients during hemoperfusion to quickly identify and manage any of these potential complications.
Comparison to Alternative Treatments
Hemoperfusion is often used in conjunction with other standard treatments. Here’s how it compares to some alternatives:
- Standard Medical Therapy: Traditional treatments for sepsis or ARDS focus on managing symptoms (e.g., antibiotics for infection, vasopressors for blood pressure). Hemoperfusion offers a more direct approach by actively removing the inflammatory molecules causing the problem.
- Dialysis (Hemodialysis/Hemofiltration): While dialysis also filters the blood, its primary function is to remove metabolic waste products and excess fluid. It is less efficient at removing larger molecules like cytokines. Hemoperfusion is often used alongside dialysis to provide more comprehensive blood purification.
- Plasma Exchange (Plasmapheresis): This procedure removes the patient’s plasma and replaces it with a substitute. While it can remove inflammatory mediators, it is less specific than hemoperfusion and also removes beneficial substances like antibodies and clotting factors.
The Future of Hemoperfusion
Research into hemoperfusion technology is ongoing. Future developments are likely to focus on creating even more selective and efficient adsorbent materials. Researchers are exploring resins that can target specific, highly pathogenic molecules while leaving beneficial components of the blood untouched.
Furthermore, as our understanding of inflammatory diseases deepens, the application of devices like the Jianfan hemoperfutor may expand. Personalized medicine approaches could one day allow clinicians to tailor hemoperfusion therapy to a patient’s specific inflammatory profile, further enhancing its effectiveness.
Final Thoughts
The Jianfan hemoperfutor represents an important advancement in the fight against life-threatening inflammatory conditions. By providing a direct method to cleanse the blood of harmful cytokines and toxins, it offers a powerful tool to support critically ill patients. While it is not a standalone cure, its ability to modulate the immune response, stabilize patients, and protect organs makes it a valuable addition to the critical care toolkit. As research continues, hemoperfusion is poised to become an increasingly integral part of modern medicine.
Frequently Asked Questions (FAQs)
Is hemoperfusion the same as dialysis?
No. While both are blood purification techniques, dialysis primarily removes small metabolic waste products (like urea) and excess water. Hemoperfusion uses adsorbent materials to remove larger molecules like cytokines and toxins, which are not effectively cleared by dialysis.
Who is a candidate for Jianfan hemoperfusion?
Candidates are typically critically ill patients suffering from conditions driven by severe systemic inflammation, such as sepsis, septic shock, or ARDS, who are not responding adequately to standard therapies.
How long does a hemoperfusion treatment last?
A single treatment session usually lasts for several hours. The total number and frequency of sessions depend on the patient’s clinical condition and the doctor’s recommendations.